Sarcopenia and Its Role in Energy Expenditure Changes
Muscle Mass Physiology and Age-Related Metabolic Shifts
Introduction
Sarcopenia—the age-related decline in skeletal muscle mass and strength—represents a primary physiological mechanism underlying altered energy balance in midlife and beyond. Progressive muscle loss beginning in the fourth decade of life contributes substantially to declining basal metabolic rate and altered body composition.
Definition and Epidemiology
Sarcopenia is characterized by:
- Progressive loss of muscle mass starting approximately age 30–40
- Accelerating decline after age 60, with estimated loss of 3–8% per decade
- Accompanied changes in muscle strength and power output
- Variability across muscle groups, with lower extremity muscles often showing greater decline
- Gender differences, with men showing greater absolute muscle loss but women potentially experiencing greater percentage decline
Population-based studies document that approximately 5–13% of individuals age 60–70 exhibit sarcopenia, increasing to 11–50% in those over 80.
Physiological Mechanisms of Muscle Loss
Scientific investigation has identified multiple mechanisms contributing to sarcopenia:
Reduced Protein Synthesis
Age-related decline in muscle protein synthetic response to protein intake and exercise stimulus, despite maintained proteasomal protein degradation.
Motor Neuron Loss
Progressive denervation of muscle fibers, particularly affecting Type II fast-twitch fibers, altering muscle fiber composition and metabolic properties.
Mitochondrial Changes
Age-related mitochondrial dysfunction and reduced oxidative capacity within muscle cells affecting energy production and muscle function.
Hormonal Influences on Muscle Mass
Multiple hormonal systems regulate muscle physiology and respond with age-related changes:
- Growth Hormone and IGF-1: Declining secretion reduces anabolic signaling for muscle protein synthesis.
- Sex Hormones: Reduced testosterone and estrogen levels contribute to altered muscle physiology in both men and women.
- Thyroid Hormones: Changes in thyroid function modulate protein metabolism and muscle turnover.
- Cortisol: Altered cortisol patterns may influence protein catabolism.
Relationship Between Muscle Mass and Energy Expenditure
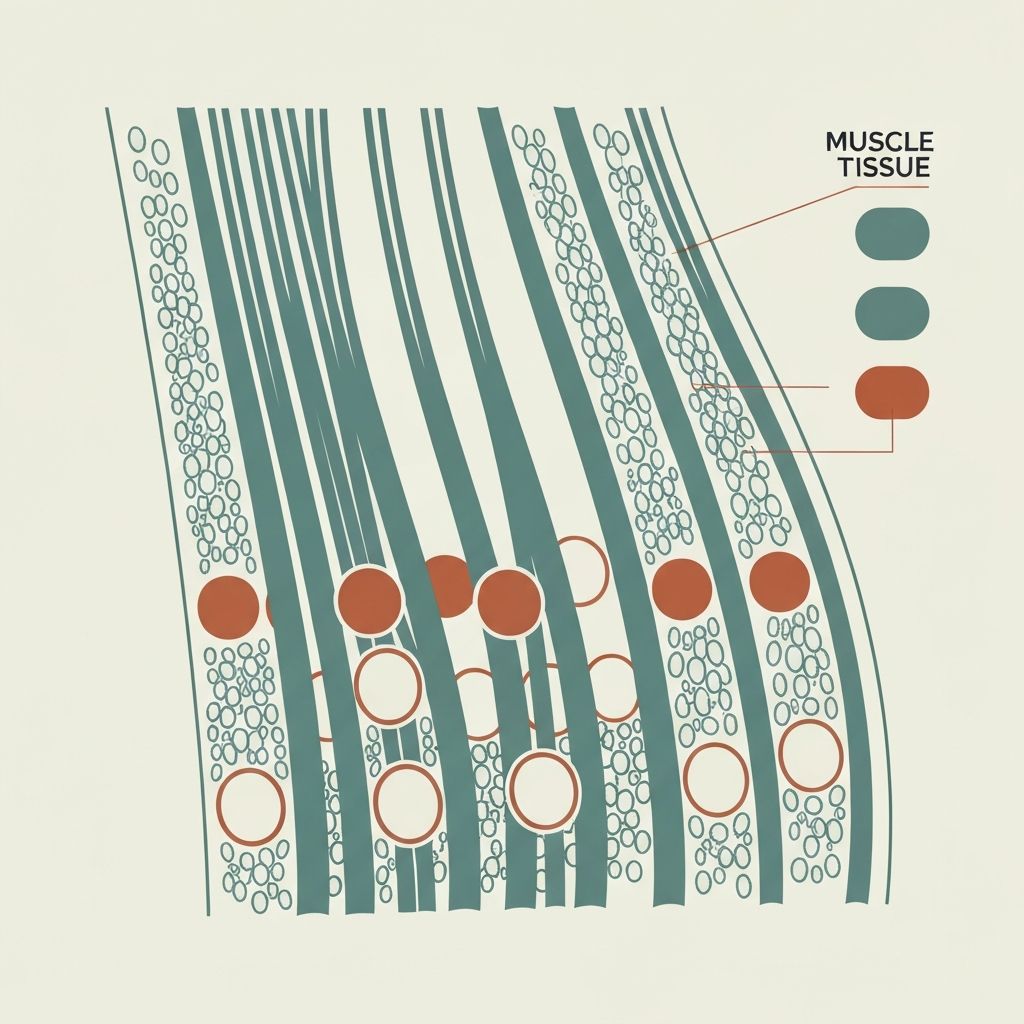
Skeletal muscle represents the primary metabolically active tissue at rest, accounting for approximately 20–30% of basal metabolic rate despite comprising 30–40% of body mass. The relationship between muscle mass and resting energy expenditure is approximately linear: each kilogram of muscle loss corresponds to approximately 4.5–5 kcal/day reduction in BMR.
Beyond resting metabolism, muscle serves as the primary site of activity-related energy expenditure, making sarcopenia particularly relevant to total daily energy expenditure decline.
Muscle Fiber Composition Changes
Age-related sarcopenia preferentially affects Type II (fast-twitch) muscle fibers, which are more metabolically active and responsive to high-intensity activity. This selective loss contributes to:
- Disproportionate loss of muscle strength relative to mass
- Reduced capacity for high-intensity physical activity
- Altered glucose metabolism and insulin sensitivity
- Changes in spontaneous activity patterns
Sarcopenia and Total Energy Balance
The consequences of sarcopenia extend beyond resting metabolism:
- Reduced Activity Thermogenesis: Declining muscle capacity reduces energy expenditure during physical activity.
- Lower NEAT: Reduced muscle mass and strength may contribute to reduced spontaneous movement.
- Altered Body Composition: Relative increase in adipose tissue, which is less metabolically active.
- Metabolic Inflexibility: Age-related changes in muscle may reduce metabolic flexibility and glucose oxidation capacity.
Individual Variation in Sarcopenia Risk
Substantial variation exists in the severity and progression of sarcopenia across individuals. Research suggests potential modulators:
- Genetic predisposition and family history of muscle loss
- Habitual physical activity patterns and exercise history
- Nutritional status, particularly protein intake
- Chronic disease burden and inflammation status
- Hormonal profile and endocrine health
Current Research Directions
Ongoing research explores interventional approaches and underlying mechanisms. Areas of investigation include molecular targets for muscle protein synthesis, exercise prescription optimization, nutritional strategies, and pharmacological interventions.
Related Topics
Explore: Age-Related Decline in Basal Metabolic Rate